Risks of Surgical Myomectomy for Fibroid Treatment
Myomectomy is a surgical procedure performed to remove uterine fibroids while preserving the uterus. It is often chosen by women who wish to alleviate fibroid-related symptoms, such as pelvic pain and heavy menstrual bleeding, while maintaining fertility. Unlike hysterectomy, which involves the removal of the uterus, myomectomy is considered a fertility-sparing option. However, like any surgical procedure, it carries certain risks that patients should carefully consider before making a decision. These risks include excessive blood loss, infection, scarring, and recurrence of fibroids, among others. This article outlines the risks associated with myomectomy, including their implications and frequency.
Excessive Blood Loss
One of the most common risks of myomectomy is excessive blood loss during surgery, particularly in patients with large or multiple fibroids. Women with fibroids often experience anemia due to heavy menstrual bleeding, which increases their susceptibility to complications related to blood loss during the procedure. In some cases, blood transfusion may be required to manage significant blood loss¹. Preoperative interventions, such as hormonal therapies or iron supplementation, are often recommended to mitigate this risk².
Infection
Postoperative infections are another concern associated with myomectomy. It is estimated that up to 5% of women may develop an infection following the procedure³. Infections can manifest as wound infections or pelvic infections and may require antibiotic treatment or, in severe cases, additional surgical intervention. Factors such as the surgical approach, duration of the procedure, and individual patient health can influence the likelihood of infection.
Formation of Scar Tissue (Adhesions)
Scar tissue formation, also known as adhesions, is a potential complication of myomectomy. Adhesions may develop in the uterus, ovaries, or surrounding organs, leading to complications such as chronic pelvic pain, bowel obstruction, or impaired fertility⁴. Intrauterine adhesions, also referred to as Asherman’s syndrome, can interfere with embryo implantation and increase the risk of miscarriage. Minimally invasive surgical techniques, such as laparoscopic myomectomy, are associated with a reduced risk of adhesion formation compared to open surgery⁵.
Damage to Surrounding Organs
During myomectomy, there is a risk of unintentional injury to nearby organs, including the bladder, intestines, and ureters. The likelihood of organ damage depends on factors such as the size and location of the fibroids and the skill of the surgeon. These injuries may require additional surgical repair and can significantly extend the recovery period⁶.
Request an Appointment
Please note that although we strive to protect and secure our online communications, and use the security measures detailed in our Privacy Policy to protect your information, no data transmitted over the Internet can be guaranteed to be completely secure and no security measures are perfect or impenetrable. If you would like to transmit sensitive information to us, please contact us, without including the sensitive information, to arrange a more secure means of communication. By submitting this form you consent to receive text messages from CVI at the number provided. Msg & data rates may apply. Msg frequency varies. Unsubscribe at any time by replying STOP.
Uterine Rupture in Future Pregnancies
Myomectomy involves incisions in the uterine wall, which can weaken its structural integrity. This weakening increases the risk of uterine rupture during future pregnancies, particularly during labor. Uterine rupture is a serious complication that can endanger the life of both the mother and the fetus. To minimize this risk, healthcare providers often recommend cesarean delivery for women who have undergone myomectomy⁷.
Recurrence of Fibroids
Myomectomy removes existing fibroids but does not prevent the formation of new ones. Studies indicate that fibroid recurrence occurs in approximately 25% to 50% of women within five years of the procedure⁸. Factors such as age, hormonal status, and genetic predisposition can influence the likelihood of recurrence. Recurrence may necessitate additional treatments, including repeat surgery.
Blood Clots
Surgical procedures, including myomectomy, can increase the risk of developing blood clots, particularly in the legs (deep vein thrombosis). If a clot travels to the lungs, it can result in a potentially life-threatening condition known as a pulmonary embolism⁹. Preventative measures, such as early mobilization and the use of compression devices, are typically employed to reduce the risk of blood clots.
Fertility Considerations
Although myomectomy is often performed to preserve fertility, the procedure itself can sometimes result in complications that impact reproductive outcomes. Scar tissue formation within the uterus may interfere with embryo implantation or increase the risk of miscarriage. Additionally, patients with extensive uterine scarring may require cesarean delivery for future pregnancies, which may influence family planning decisions¹⁰.
Anesthesia Risks
Like all surgeries requiring anesthesia, myomectomy carries certain risks related to the use of anesthesia, such as allergic reactions, respiratory issues, and cardiovascular complications. These risks are generally low and are carefully managed by the anesthesiology team during the procedure¹¹.
Prolonged Recovery Time
Recovery time following myomectomy depends on the surgical approach. Abdominal myomectomy typically requires a longer recovery period (four to six weeks) compared to minimally invasive techniques, such as laparoscopic or hysteroscopic myomectomy, which have shorter recovery times (two to four weeks). Prolonged recovery can affect daily activities and work commitments, making it an important consideration for patients when deciding on treatment options¹².
Uterine Fibroid Embolization: A Lower-Risk Alternative
For women seeking a less invasive alternative to myomectomy, uterine fibroid embolization (UFE) offers a lower-risk option. UFE is a minimally invasive procedure performed by our interventional radiologist, where tiny particles are injected into the uterine arteries to block the blood flow to fibroids, causing them to shrink. Unlike myomectomy, UFE eliminates the need for major surgery, reducing risks such as excessive blood loss, infection, and prolonged recovery time. Studies have shown that UFE has a high success rate in relieving fibroid-related symptoms, without the need for hospital stays and faster recovery compared to surgical interventions¹³. Furthermore, UFE avoids the risks of surgical adhesions and organ damage, making it an attractive option for many women.
Uterine Fibroid Embolization (UFE)
UFE can help you get your life back without any scarring or hospital stay. It can reduce the size of your fibroids, relieve your symptoms, and retain your fertility. Most women can return to their normal activities in two to seven days.
How is the UFE performed?
- You will receive twilight sedation to help you relax
- Our specialist numbs the skin on the wrist or groin
- A tiny catheter is placed
- Small beads are placed into the fibroid artery
- The catheter is removed
- Band-Aid is applied
- Recover at home
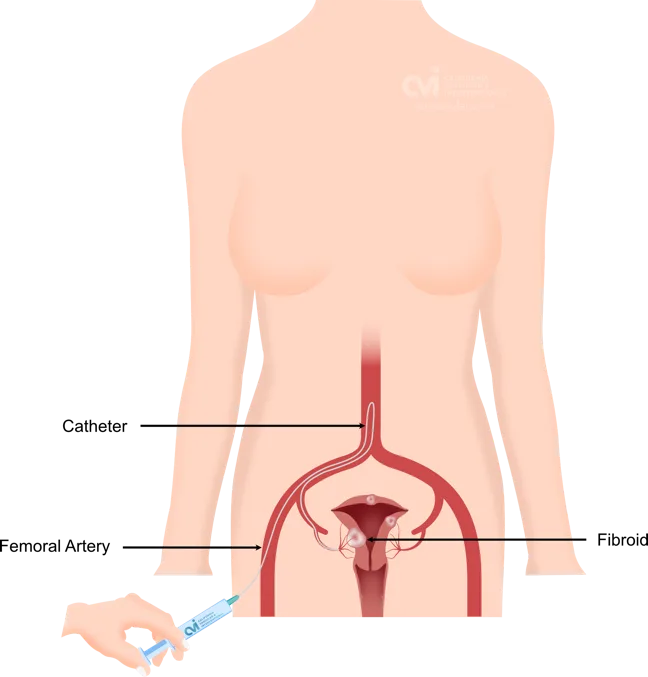
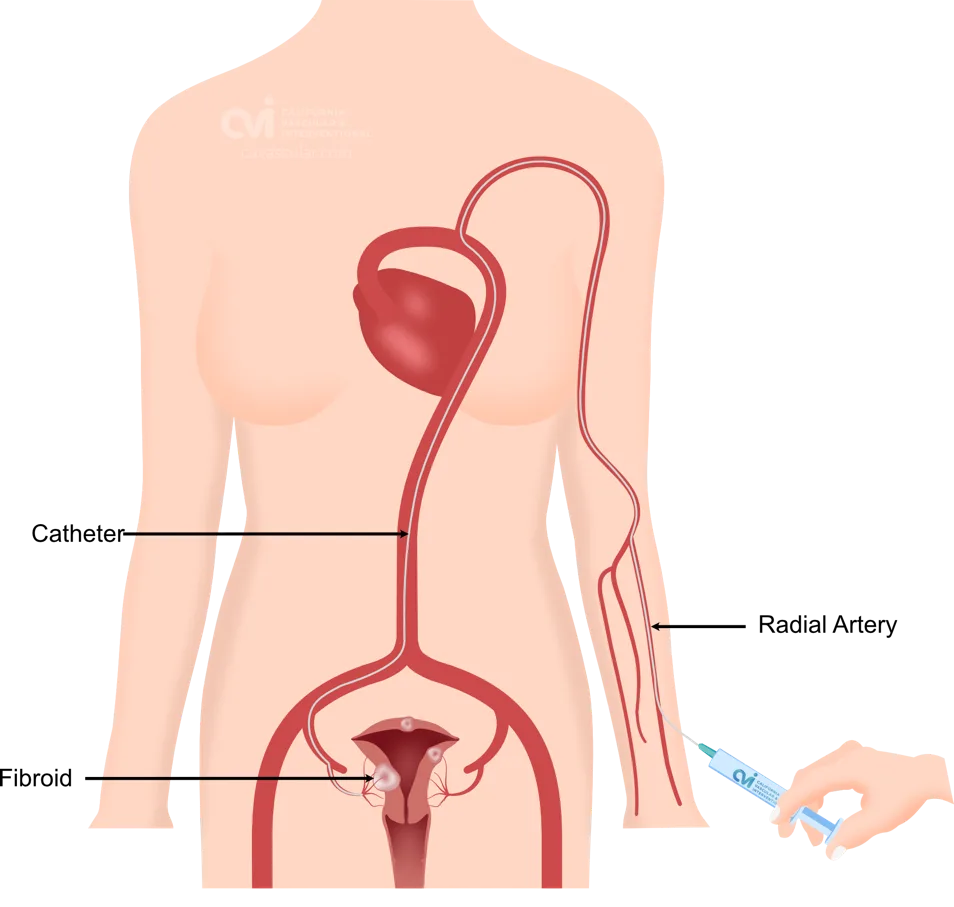
The patient is given a local and topical anesthetic to numb the skin and a mild sedative, so that the procedure is not painful.
Some of the UFE advantages include:
- No hospital stay
- No general anesthesia
- No stitches
- No blood loss
- No risk of hysterectomy
- No major scars
- No surgical risks
Why California Fibroid Center?
At CVI, we provide devoted and specialized care for embolization. Our doctor is a double board-certified doctor who specializes in image guided treatments and embolizations. Dr Allaei not only has an experience in treating many routine patients with different sized uterine fibroids and adenomyosis, but also treats complex cases, prior treatment failures as well as women who are post-menopausal. This has allowed many patients to undergo embolization procedures no matter the complexity safely with outstanding results. As an expert in his field having performed over 5,000 image-guided treatments, patients receive top care in expert hands. The staff are also highly trained and dedicated to the patient experience. This allows us to provide the best care and experience for our patients.
Women continue to be thrilled with the totality of their care experience facilitated by our patient-centered approach. Get your procedure done right the first time.
Patient Centered. Dedicated. Comprehensive.
Is Myomectomy right for me?
While myomectomy is a valuable surgical option for women seeking relief from fibroid symptoms while preserving fertility, it is not without risks. These risks include excessive blood loss, infection, adhesion formation, damage to surrounding organs, uterine rupture in future pregnancies, recurrence of fibroids, blood clots, fertility considerations, anesthesia-related complications, and prolonged recovery time. Patients considering myomectomy should have a detailed discussion with a fibroid specialist about these risks and alternative treatment options to make an informed decision. By understanding the potential complications and their implications, patients can better weigh the benefits of myomectomy against the associated risks.
Have More Questions?
We are Here to Help
Request an appointment to meet with our fibroid specialist who will review your imaging, labs and history to determine if you are candidate for the procedure, and the outcomes you can expect. Each woman is an individual and should discuss the potential risks and benefits of fibroid embolization and other Treatments with our doctor to decide which option is best for her.
Appointments are available via an online video telehealth platform or in person at one of the offices in Los Angeles, Orange County or San Diego. Why should you choose us? Read here.
1. Parker WH. Uterine myomas: Management. Fertility and Sterility. 2007;88(2):255-271. doi:10.1016/j.fertnstert.2007.06.002
2. Mayo Clinic. Myomectomy: What you can expect. https://www.mayoclinic.org
3. UCSF Health. Myomectomy Overview. https://www.ucsfhealth.org
4. Tulandi T, Al-Fozan H. Adhesion prevention in gynecologic surgery. Obstetrics & Gynecology Clinics of North America. 2003;30(3):567-584. doi:10.1016/s0889-8545(03)00064-6
5. Chapron C et al. Uterine adhesions after laparoscopic myomectomy: Prevention and impact on fertility. Human Reproduction. 2001;16(8):1720-1723. doi:10.1093/humrep/16.8.1720
6. American Society for Reproductive Medicine. Complications of fibroid surgery. https://www.asrm.org
7. Guven ES, Camus M. Reproductive impact of myomectomy. Best Practice & Research Clinical Obstetrics & Gynaecology. 2008;22(4):749-759. doi:10.1016/j.bpobgyn.2008.01.007
8. Friedman AJ, Barbot J, Gleason RE. Recurrence of fibroids after myomectomy. Obstetrics & Gynecology. 1985;65(3):391-395.
9. Better Health Channel. Myomectomy risks. https://www.betterhealth.vic.gov.au