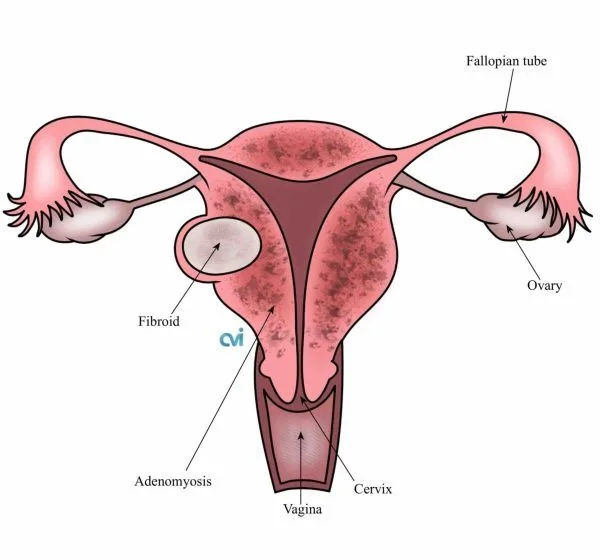
What is adenomyosis?
Adenomyosis is a benign uterine condition in which the uterine lining (endometrium) grows into the muscular wall of the uterus, leading to heavy menstrual bleeding, painful periods, pelvic pressure, bloating, and fatigue. Adenomyosis may be diffuse, involving large areas of the uterus, or focal, affecting a more localized region.¹
The two main approaches are surgery and uterine artery embolization (UAE), although a lot of patients are never told about the uterus preserving UAE option. Understanding the benefits, risks, and long-term consequences of each is essential—especially for patients hoping to preserve their uterus or avoid major surgery. Patients must advocate for themselves and research options, since doctors may only present their own services.
Surgical Treatment: Hysterectomy for Adenomyosis
A hysterectomy, or removal of the uterus, is traditionally offered by GYNs as the definitive surgical treatment for adenomyosis and is often recommended for patients with severe symptoms who do not desire future pregnancy. ²
Although hysterectomy eliminates uterine bleeding and pain, this is major pelvic surgery and has important long-term consequences that are often under-discussed. ²

Pelvic floor instability after hysterectomy
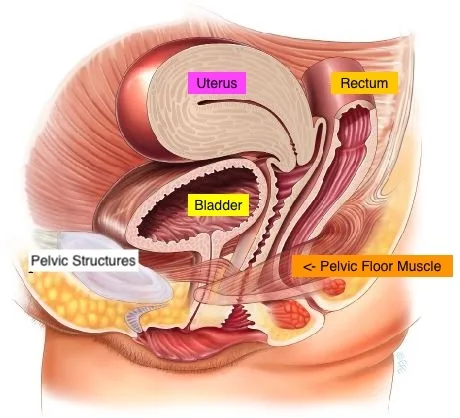
The uterus plays a key role in the body besides pregnancy.
It is the central structure in pelvic floor support, as it is connected to the pelvis by ligaments that help maintain normal anatomy of the bladder, vagina, and rectum. Removal of the uterus disrupts these ligaments and alters pelvic biomechanics.³ It was never meant to be removed once pregnancy is no longer needed.
Multiple large studies have shown that hysterectomy is associated with an increased risk of pelvic organ prolapse, including vaginal vault prolapse, bladder prolapse (cystocele), and rectal prolapse (rectocele).³⁻⁴ Prolapse essentially means these organs drop downward from their normal position protruding into the vagina.
Long-term data suggest that up to 10–20% of women will require treatment for pelvic organ prolapse after hysterectomy, depending on age, surgical technique, and prior pelvic floor strength.⁴⁻⁵
Need for pessaries and pelvic support devices
Because of pelvic floor instability after hysterectomy, a significant number of patients eventually require pessaries or other vaginal support devices to manage symptoms such as pressure, bulging, urinary leakage, or difficulty with bowel movements.⁵
Population-based studies estimate that approximately 8–15% of women will use a pessary or undergo additional pelvic floor interventions following hysterectomy during long-term follow-up.⁵
Some patients ultimately require additional pelvic reconstructive surgery, particularly as they age or if they have risk factors such as obesity, chronic coughing, or prior vaginal deliveries.⁴⁻⁵

Other surgical risks
In addition to pelvic floor issues, hysterectomy carries risks including:
- Bleeding and blood transfusion
- Infection
- Injury to bladder, bowel, or ureters
- Blood clots
- Anesthesia complications
- Longer recovery time compared with minimally invasive procedures²
If you want to avoid a hysterectomy and potential risks and long term issues, a non-surgical UAE option is offered. Read more below.
Surgical Treatment: Adenomyomectomy
For patients wishing to preserve the uterus, adenomyomectomy involves surgically removing the adenomyosis tissue while reconstructing the uterine muscle. This is most successful in focal adenomyosis and technically challenging in diffuse disease.⁶
This is a complex surgery as the tissue is intertwined with the uterine muscle and not simple to dissect apart resulting in high operative bleeding. Pregnancy rates after surgery average about 53% for focal adenomyosis and 34% for diffuse adenomyosis.⁷ Also, pregnancy after adenomyomectomy is considered high risk, with reported cases of uterine rupture, particularly in diffuse disease.⁷⁻⁸ Recurrence remains possible, with a pooled recurrence rate of approximately 13% after surgery.⁹
In a survey-style study on adenomyosis management, an adenomyomectomy was offered by about 24% of respondents overall—meaning roughly 1 in 4 clinicians said they would offer it.¹ What this means in plain English: most patients will not be offered adenomyomectomy at a typical general OB-GYN practice. Even among surgeons who technically “offer” adenomyomectomy, high-volume experience is less common. Why isn’t it more common? Adenomyomectomy can be technically demanding, make many clinicians steer patients either toward UAE (uterus-sparing, minimally invasive) or hysterectomy (definitive), depending on goals and severity.
Request an Appointment
Please note that although we strive to protect and secure our online communications, and use the security measures detailed in our Privacy Policy to protect your information, no data transmitted over the Internet can be guaranteed to be completely secure and no security measures are perfect or impenetrable. If you would like to transmit sensitive information to us, please contact us, without including the sensitive information, to arrange a more secure means of communication. By submitting this form you consent to receive text messages from CVI at the number provided. Msg & data rates may apply. Msg frequency varies. Unsubscribe at any time by replying STOP.
Non-Surgical Treatment: Uterine artery embolization (UAE) for Adenomyosis
What is UAE?
Uterine artery embolization (UAE) is a non-surgical, image-guided procedure that reduces blood flow to the adenomyosis tissue, leading to shrinkage and symptom relief while preserving the uterus.¹⁰
Effectiveness of UAE
A major systematic review showed that approximately 80–85% of patients experience significant improvement in bleeding and pain after UAE for adenomyosis.¹⁰
Importantly, UAE has been shown to be effective in diffuse adenomyosis, where surgery is often difficult or carries higher risk.¹⁰
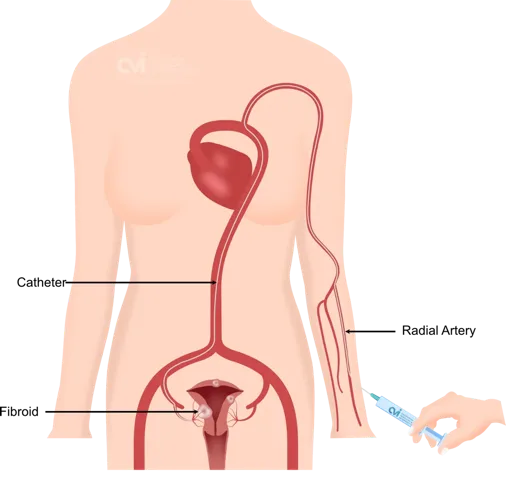
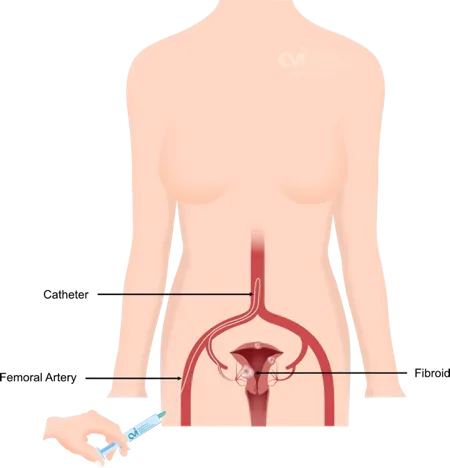
How is the UFE Procedure Performed?
- You will receive twilight sedation to help you relax
- Our specialist numbs the skin on the wrist or groin
- A tiny catheter is placed
- Small particles are placed into the fibroid artery
- The catheter is removed
- Band-Aid is applied
Recover at home
Recurrence and repeat treatment
Because the uterus remains in place, symptoms may recur in some patients. A 2023 meta-analysis found a recurrence rate of approximately 30% after UAE, though many patients still avoid hysterectomy long term.⁹
Fertility considerations after UAE
Pregnancy after UAE has been reported, including successful full-term deliveries.¹¹ While fertility data are still evolving, UAE offers a uterus-sparing alternative for patients who are not ideal surgical candidates or who wish to avoid the risks of uterine incision and reconstruction.¹¹
Risks of UAE
Potential risks include:
- Post-procedure cramping and fatigue
- Temporary flu-like symptoms
- Infection (rare)
- Vascular access complications
- Very rare non-target embolization¹⁰
Recovery is faster than surgery, with patients resuming normal activities within 1 week at the California Fibroid Center.¹⁰
Surgery vs. UAE: patient-centered perspective
Because hysterectomy permanently alters pelvic anatomy and increases long-term pelvic floor risks, many experts consider uterus-sparing options such as UAE before hysterectomy, particularly when symptoms can be controlled without removing the uterus.²⁻⁵
For many patients, hysterectomy should be viewed as a last-resort option, reserved for those who have failed less invasive therapies or who fully understand the long-term pelvic consequences.
Why California Fibroid Center?
Dr. Allaei and the team at California Fibroid Center have extensive experience treating adenomyosis using uterine artery embolization, including complex diffuse disease and cases combined with fibroids. The center is recognized for its high procedural volume in UAE and advanced image-guided care, allowing patients to pursue a non-surgical, uterus-preserving option before considering hysterectomy.¹²
Have More Questions?
We are Here to Help
Request an appointment to meet with our fibroid specialist who will review your imaging, labs and history to determine if you are candidate for the procedure, and the outcomes you can expect. Each woman is an individual and should discuss the potential risks and benefits of fibroid embolization and other Treatments with our doctor to decide which option is best for her.
Appointments are available via an online video telehealth platform or in person at one of the offices in Los Angeles, Orange County or San Diego. Why should you choose us? Read here.
- Van den Bosch T, et al. Ultrasound Obstet Gynecol. 2019.
- SOGC Guideline No. 437. J Obstet Gynaecol Can. 2023.
- Hendrix SL, et al. Pelvic organ prolapse after hysterectomy. Obstet Gynecol. 2002.
- Altman D, et al. Risk of pelvic organ prolapse surgery after hysterectomy. Lancet. 2007.
- Wu JM, et al. Lifetime risk of pelvic floor surgery. Am J Obstet Gynecol. 2014.
- Grimbizis GF, et al. Hum Reprod Update. 2014.
- Tan J, et al. Fertil Steril. 2018.
- Sayama S, et al. J Obstet Gynaecol Res. 2023.
- Liu X, et al. Obstet Gynecol. 2023.
- 10. de Bruijn AM, et al. J Vasc Interv Radiol. 2017.
- Popovic M, et al. AJR Am J Roentgenol. 2011.
- California Fibroid Center / California Vascular & Interventional – clinical experience data.